Is Fibromyalgia a Mitrochondrial Disorder?
Reprinted with permission from Cort Johnson and Health Rising.
We tend to think of fibromyalgia as a central nervous system disease but that focus has tended to obscure the growing evidence of problems in the body.
We don’t tend to think of fibromyalgia as an inflammatory disorder. It’s true that overt signs of inflammation are rarely found in people with FM, but some studies suggest inflammatory factors may play a role.
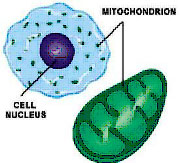
Then there are the mitochondria. Mitochondrial dysfunction is thought of as a real possibility in chronic fatigue syndrome, but I’ve rarely associated it with fibromyalgia or pain. It turns out, however, that multiple studies – most of them small – suggest that mitochondrial dysfunction could indeed play a significant role in fibromyalgia.
Could fibromyalgia, whatever else it is – also be a mitochondrial disorder?
A Mitochondrial Disorder?
Studies suggest the energy factories may be running a bit low in FM. Muscle biopsies have found patterns of mitochondrial dysfunction (abnormal mitochondria, mitochondrial defects and muscle fiber abnormalities) similar to those typically found in mitochondrial disorders. Some skin biopsies have shown patterns of neurogenic inflammation and oxidative stress – two factors that negatively impact the mitochondria. Peripheral blood cells have demonstrated CoQ10 deficiency, mitochondrial dysfunction, oxidative stress and mitochondrial degradation.
In 2013 a Spanish group proposed that mitochondrial dysfunction in FM patients was driving an inflammatory process. Now, in 2015 they have returned with a study looking at mitochondrial dysfunction, oxidative stress and inflammation using skin biopsies from people with FM.
Given the allodynia present and the increasing evidence of small fiber neuropathy in FM, the skin is becoming an ever more intriguing place to look in fibromyalgia. Something, after all, is “burning away” those small unmyelinated nerve fibers in their skin. Is it inflammation? Are the mitochondria going bananas? (Could it be both?) This study won’t tell us what’s causing the SFN or allodynia in FM – it’s not going to assess either of them – but it may provide some suspects future studies can follow up on.
This small Spanish study looked at the levels of mitochondrial enzymes, mitochondrial proteins, ATP, CoQ 10 and TNF-a from a small patch of skin in the left shoulder region, as well as in the blood and saliva of 23 people with FM and 20 healthy controls.
A Mitochondrial Disorder
Significant reductions in mitochondrial enzyme activity (in complexes I, II, III and IV) were found in the FM patients but not the healthy controls. That, in combination with reduced levels of mitochondrial proteins, indicated that mitochondrial functioning was indeed significantly reduced. So were CoQ10 and ATP levels and mitochondrial DNA levels. In fact, every aspect of mitochondrial functioning tested was found to have taken a significant hit in the FM patients.
That suggested mitochondrial damage had occurred and that finding set the stage for the next test. Since damaged mitochondrial DNA are known to spark an inflammatory response, the researchers asserted they should also be able to find evidence of inflammation in the skin – and they did. Double the levels of the pro-inflammatory cytokine TNF-a were found in the skin of the FM patients.
Not only were the increased cytokine levels strongly associated with reduced mtDNA – suggesting that the mitochondrial problems had indeed sparked the inflammation – but they were highly correlated with the pain levels in FM (p<.001) as well. That suggested the mitochondrial problems could be causing or contributing to the pain the FM patients were experiencing.
A threefold increase in TNF-a levels in the saliva and the blood collected from the biopsy area relative to the healthy controls suggested that widespread or systemic inflammation and oxidative stress was present as well. The FM patients looked pretty much like a soup of mitochondrial dysfunction, oxidative stress and inflammation.
The Pain, Inflammation and….Mitochondrial Disorders?
They are not alone. A similar situation appears to apply in diabetic patients with peripheral neuropathy and/or allodynia. Low levels of mitochondria have also been associated with small fiber neuropathy – a condition that appears to occur in about 40% of people with fibromyalgia.
Cancer associated pain displays some similarities as well. The sensory and autonomic nerves appear to be primarily affected in both cancer pain and FM. Pro-inflammatory cytokines, oxidative stress, mitochondrial damage/dysfunction, dorsal root ganglia, central sensitization, immune activation, and possibly microglial activation have been implicated in both as well.
Some models of cancer pain mimic the pain model proposed in this paper – mitochondrial dysfunction sparking an innate immune response that ends up damaging the peripheral nerves.
Cancer pain researchers are looking at novel treatments to undo this mitochondrial/inflammatory mess. They include ways to block peroxynitrite and heat shock proteins, using minocycline, an antibiotic, to attenuate activated microglia, and adenosine receptor agonists to protect the nerves. If mitochondrial dysfunction does induce pain in cancer, any of the above could ultimately show up as a treatment option for FM patients.
Chicken or the Egg?
Whether mitochondrial dysfunction is causing inflammation or inflammation is knocking out the mitochondria is unclear, however. The fact that anti-inflammatory drugs have not generally been found to be particularly effective in FM argues against an inflammatory origin. (The right types of anti-inflammatories, however, may not have been tested.)
Several studies, on the other hand, suggest that mitochondrial enhancers such asCoQ10 may be helpful in reducing the pain and headache symptoms in FM, and some practitioners have had good results with D-Ribose in ME/CFS and/or FM.
CoQ10 is a particularly intriguing nutrient given its ability to both boost ATP production and reduce levels of oxidative stress. C0Q10 levels are reportedly low in many neurodegenerative disorders including Parkinson’s disease, diabetes, fibromyalgia and cancer.
A fibromyalgia study by this Spanish research group found a 50% reduction in COQ10 levels in FM. With dozens of mostly small studies examining mitochondrial dysfunction and CoQ10 levels/supplementation in FM and other disorders under it’s belt, this Spanish research group has been leading the way in this area.
On the ME/CFS side, Maes has been producing review papers and studies on oxidative stress, mitochondrial functioning and inflammation for years. Presentations on the exercise problems in ME/CFS at the IACFS/ME Conference also appeared to be pointing an arrow at the mitochondria.
Interest in the mitochondria appears to be, er, powering up. Dr. Klimas’s Institute of Neuro Immune Medicine at Nova Southeastern University recently engaged a mitochondrial expert. The Chronic Fatigue Initiative’s announcement that they’re going to be digging into the mitochondria suggests we may get some much-needed high-powered studies into the field.
The results of one such study – the multi-center Synergy trial in chronic fatigue syndrome – that’s been testing the effectiveness of a low-dose stimulant in combination with mitochondrial and immune enhancing supplements in ME/CFS – should be out around mid-year.
Stay tuned.
_______________
About the Author: Cort Johnson has had ME/CFS for over 30 years. The founder of Phoenix Rising and Health Rising, Cort has contributed hundreds of blogs on chronic fatigue syndrome, fibromyalgia and their allied disorders over the past 10 years. Find more of Cort's and other bloggers' work at Health Rising.





