Fibromyalgia: The Stigma and the Truth
 "Fibromyalgia: The Stigma and the Truth"
"Fibromyalgia: The Stigma and the Truth"
Reprinted with permission from Washington Post Communities Digital News
Written by Paul Mountjoy
WASHINGTON- January 24, 2014—Those suffering from fibromyalgia syndrome (FMS) now have undeniable proof that their illness is not psychogenic or psychosomatic (in the mind), thanks to a plethora of new and current findings from the most respected medical research facilities in the U.S.A.
After years of being ignored and told that it was all in their minds, like individuals suffering from obesity before them, FMS sufferers are finally getting the acknowledgment they deserve.
Denied the recognition, compassion and disability benefits they so desperately needed, until recent research emerged, FMS sufferers were subjected to skepticism by family members, employers, friends and the legal profession. Even many primary care physicians turned a deaf ear to FMS sufferers.
Isolated and trapped into forced silence by negative reactions to their ailment, FMS victims were often overcome by fear of asking medical practitioners to address their symptoms and fear of asking family members for help in their day-to-day lives.
The disdain suffered by many with FMS exacerbated the depression they were already experiencing as a result of the condition.
The general confusion surrounding FMS among the medical and other professions may lie in the syndrome’s etiology, the cause or set of causes that gives rise to a disease or condition. Currently, research has been unable to identify a single, specific cause that leads to FMS; instead, FMS appears to have multiple sources of causation.
FMS and Obesity: A Comparison
The attitudes toward FMS are analogous to traditional attitudes toward obesity.
Historically, it was believed that those who were overweight were lazy overeaters with poor self-control. Friends, family and healthcare professionals advised more exercise and less food. While poor diet and inadequate exercise are the predominant reasons for body weight issues, hundreds of thousands of overweight people are as active as their slimmer counterparts, and in many cases eat less.
Fortunately for some with ‘metabolic syndrome’ —the medical term used to describe patients with weight problems—medical research has finally produced answers. The good news is that in many cases weight problems and obesity arise form a genetic disorder that makes the condition difficult if not impossible to overcome. Dr. Jeremy Cooke maintains there are individuals so genetically predisposed to obesity that they may never lose or keep weight off.
The bad news is that obesity may not be closely linked to individual lifestyle and dietary choices, which can make many individuals’ life-long battle with weight issues a war without victory. Even for those who do not have a genetic predisposition to having weight problems, being overweight may be attributed to factors other than laziness and overeating. Prolonged increased levels of stress, which cause the release of certain hormones from the hypothalamic-pituitary-adrenal axis, for example, can cause metabolic syndrome.
Aging, genetics, accumulation of stress hormones, sleep issues and several other factors not related to activity or diet can also cause metabolic syndrome. These in turn may lead to diabetes, coronary issues, high blood pressure, chronic pain, depression, stress and a host of other related health problems.
Thanks to the identification of metabolic syndrome as a disease, however, sufferers are no longer called lazy, inactive or just plain “fat” by friends, family, and the medical profession.
Before obesity was identified as a legitimate disease, the emotionally pervasive level of frustration felt by those suffering from it was similar to what victims of FMS are currently experiencing.
There are a number of other similarities between FMS and metabolic syndrome. A single cause has not been identified for either FMS or metabolic syndrome, and it is believed that there are several if not many causes that lead to both syndromes. The resulting symptoms of both are extensive and varied, and the effect of both on health is severe, undeniable and not psychogenic.
FMS as a Syndrome
”Syndrome” is defined as a group of symptoms that consistently occur together or a condition characterized by a set of associated symptoms that cause an abnormal physiological condition. This definition is the hallmark of FMS.
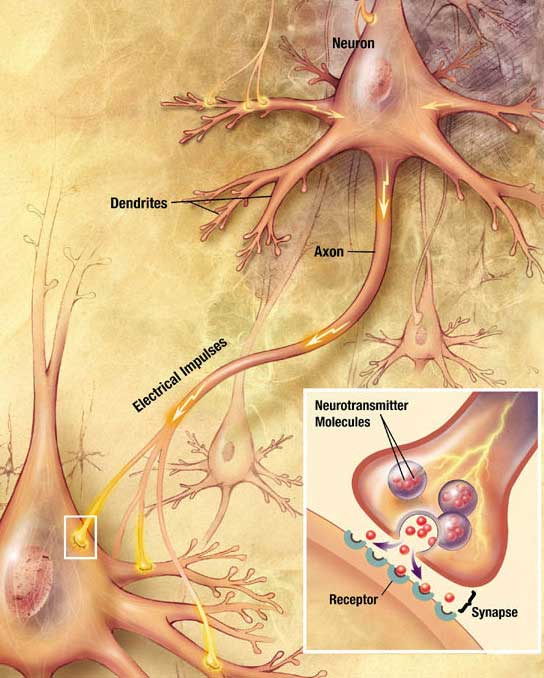
The causes of FMS range from sleep issues, to central nervous system damage, peripheral nervous system problems, hormonal imbalances and serotonin concerns, all of which may have serious implications.
For example, central nervous system damage may arise from injury, causing disrupted pain processing. Peripheral nervous system problems such as blocked AV shunts can cause an array of pain and body temperature problems. Hormonal imbalances involve hypothalamus-pituitary and thyroid gland functions, and serotonin problems include poor production and inhibited serotonin reuptake.
A variety of treatments are available for FMS, yet each treatment must be individualized to address its particular causes. For example, serotonin may be a primary factor for some patients’ FMS, while endocrine system imbalance or injury may the primary cause for others. For this reason, one single specific treatment is not appropriate to treat all forms of FMS.




