Brain Signal Disruption for Pleasure and Pain in Fibromyalgia Patients
Hyperalgesia, or increased pain sensitivity, is higher in people with fibromyalgia, and research shows that disrupted brain signals for reward and punishment may be a contributing factor.
The study results published in Arthritis & Rheumatism, a journal of the American College of Rheumatology, suggest that this altered brain processing might contribute to widespread pain and lack of response to opioid therapy in patients with fibromyalgia.
In a press release from Wiley, publisher of Arthritis & Rheumatism, lead author Dr. Marco Loggia from Massachusetts General Hospital and Harvard Medical School in Boston is quoted as saying, “In patients with fibromyalgia there is an alteration in the central nervous system pain processing and a poor response to topical pain treatments, trigger point injections and opioids. Our study examines the disruption of brain function involved in the individual experience of pain anticipation and pain relief.”
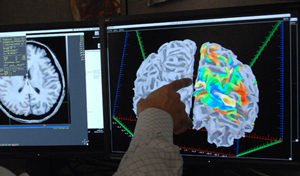
Fibromyalgia patients showed less brain activity in regions involved with sensory, affective, cognitive and pain regulating processes during pain anticipation and relief. The study of 31 patients with fibromyalgia and 14 controls used fMRI, cuff pressure stimuli on the leg, and visual cues during the fMRI of impending pain onset (anticipation) and pain offset (relief anticipation). In healthy controls, the center of the brain processing reward and punishment was activated during pain anticipation and stimulation and deactivated during anticipation of relief. In fibromyalgia patients, the brain responses during pain, and anticipation of pain and relief, were significantly reduced or inhibited.
Dr. Loggia concluded, “Our findings suggest that fibromyalgia patients exhibit altered brain responses to punishing and rewarding events, such as expectancy of pain and relief of pain. These observations may contribute to explain the heightened sensitivity to pain, as well as the lack of effectiveness of pain medications such as opioids, observed in these patients. Future studies should further investigate the neurochemical basis underlying these dysfunctions.”
This research was supported by the National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health (NIH) grants (R01-AT004714, P01- AT002048, P01-AT006663, R01-AT005280; R01-AG034982, R21-AR057920).






